The healthcare industry is undergoing a transformation, and remote patient monitoring (RPM) is at the forefront of this evolution. As we approach 2025, the demand for RPM solutions is surging, driven by advancements in technology and the growing need for accessible, patient-centered care. However, turning innovative RPM ideas into reality requires significant funding, a challenge many startups face.
Understanding how to secure capital for RPM initiatives is crucial for healthcare entrepreneurs. A broader funding perspective is provided in how to secure funding for healthcare startups, offering a contextual backdrop that complements your exploration of remote patient monitoring capital strategies. This blog will delve into innovative funding approaches, including federal grants, reimbursement models, and strategic partnerships, to help RPM startups thrive in 2025.
RPM Funding Opportunities and Sources
Remote patient monitoring (RPM) funding has evolved into a dynamic landscape, offering healthcare providers and organizations a variety of avenues to secure financial support. From federal and state grants to Medicare reimbursements and private funding, the opportunities are vast and growing. This section explores these funding sources, highlighting key trends and actionable insights for maximizing RPM investments.
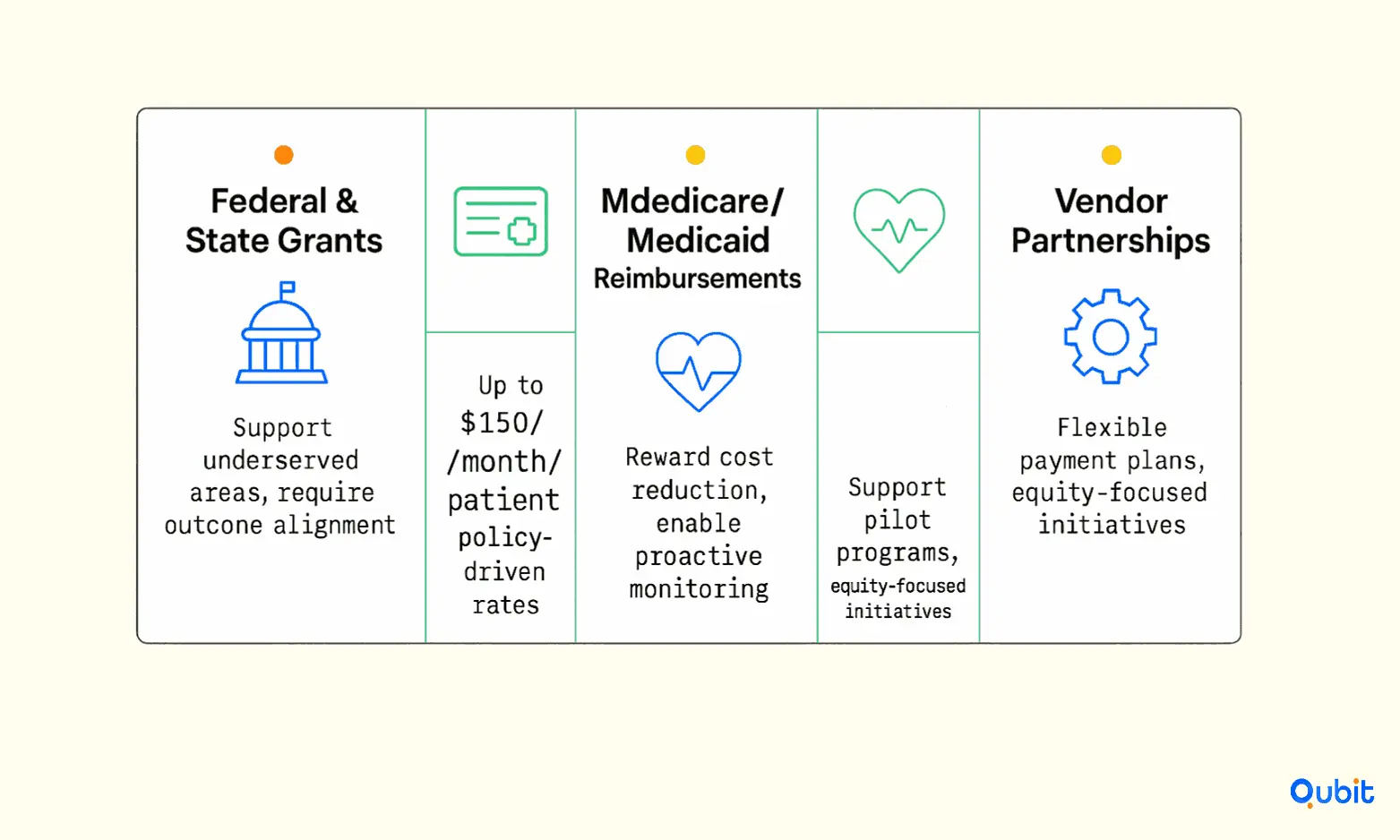
Federal and State Grant Programs
Government-backed grants are a cornerstone of RPM funding, providing essential financial support for innovative healthcare initiatives. Federal grants for RPM often target underserved populations, rural areas, and chronic disease management programs. For example, the Health Resources and Services Administration (HRSA) offers grants aimed at expanding telehealth and RPM services in rural communities. Similarly, state-level programs frequently align with federal initiatives, offering complementary funding to enhance accessibility and adoption.
To secure these grants, organizations must demonstrate measurable outcomes, such as improved patient engagement or reduced hospital readmissions. By aligning proposals with government priorities, healthcare providers can tap into substantial funding pools to expand their RPM capabilities.
Medicare and Medicaid Reimbursements
Medicare and Medicaid reimbursements have become pivotal in sustaining RPM programs. The growth in traditional Medicare RPM spending, from $6.8 million in 2019 to $194.5 million in 2023, underscores the increasing reliance on these reimbursements. Additionally, RPM claim volumes surged by an impressive 1,294%, reflecting heightened adoption across the healthcare sector.
Recent policy changes have introduced new RPM codes with reimbursement rates ranging between $120 and $150 per patient monthly. These updates incentivize providers to integrate RPM into their care models, ensuring financial viability while improving patient outcomes. For Medicaid, state-specific policies often dictate reimbursement rates, requiring providers to stay informed about local regulations to optimize funding opportunities.
Value-Based Care Models
The shift toward value-based care has opened new doors for RPM funding. By focusing on outcomes rather than service volume, value-based care models reward providers for reducing costs and improving patient health. RPM plays a critical role in achieving these goals, offering real-time data and proactive interventions that prevent costly complications.
Organizations participating in Accountable Care Organizations (ACOs) or bundled payment programs can leverage RPM to meet performance metrics and unlock additional funding. For example, RPM can help reduce hospital readmissions, a key metric in many value-based care agreements, while enhancing patient satisfaction scores.
Private and Nonprofit Funding
Private grants and nonprofit organizations also contribute significantly to RPM funding. Foundations like the Robert Wood Johnson Foundation and the Commonwealth Fund often support projects that align with their mission to improve healthcare access and equity. These grants can be particularly useful for pilot programs or initiatives targeting specific populations, such as seniors or individuals with chronic conditions.
Private funding sources, including venture capital and corporate sponsorships, are increasingly drawn to RPM due to its scalability and potential for long-term cost savings. Healthcare providers can attract these investors by showcasing the financial and clinical benefits of their RPM programs, supported by robust data and success stories.
Technology Vendor Partnerships
Collaborations with technology vendors offer another avenue for RPM funding. Many vendors provide financial assistance or flexible payment plans to help healthcare organizations adopt their solutions. These partnerships often include training, technical support, and integration services, reducing the upfront costs associated with RPM implementation.
In addition, vendors may offer performance-based pricing models, where payments are tied to the achievement of specific outcomes, such as reduced emergency room visits or improved patient adherence. This approach aligns financial incentives with clinical goals, fostering mutually beneficial relationships between providers and vendors.
Key funding patterns align with observations in telehealth funding outlook, where evolving market projections enhance your understanding of supportive trends in remote patient monitoring.
Actionable Steps for Securing RPM Funding
To maximize funding opportunities, healthcare providers should:
1. Research Available Grants: Explore federal, state, and private grant programs that align with your RPM goals.
2. Optimize Reimbursement Strategies: Stay updated on Medicare and Medicaid policies to ensure compliance and maximize reimbursements.
3. Adopt Value-Based Care Models: Integrate RPM into care models that reward outcomes, such as ACOs or bundled payment programs.
4. Engage with Nonprofit Organizations: Partner with foundations that support healthcare innovation and equity.
5. Collaborate with Vendors: Negotiate partnerships that reduce upfront costs and align financial incentives with clinical outcomes.
By diversifying funding sources and staying informed about emerging trends, healthcare providers can build sustainable RPM programs that deliver both financial and clinical benefits.
Key Drivers for Capital Raising in RPM
Securing Funding for RPM Implementation
Implementing remote patient monitoring (RPM) programs requires a well-rounded funding strategy that combines public and private resources. By integrating federal grants, reimbursements, private investments, and vendor partnerships, healthcare organizations can establish sustainable RPM systems that enhance patient care while generating consistent revenue.
1. Utilize Federal Grants for Initial Investment
Federal grants are a critical starting point for RPM funding. Programs such as the Federal Communications Commission (FCC) telehealth grants provide substantial financial support for technology acquisition and program development. For example, the Community Health Center of Southeast Kansas (CHC/SEK) secured $366,167 through FCC telehealth grants, enabling them to implement RPM devices from CareSimple and reach over 3,000 patients. Healthcare organizations should actively monitor grant opportunities and submit detailed proposals that emphasize the program’s potential to improve patient outcomes and reduce healthcare costs.
2. Maximize Medicare RPM Reimbursements
Medicare reimbursements offer a reliable revenue stream for RPM programs. By adhering to Medicare’s guidelines for remote patient monitoring services, healthcare providers can generate over $1,000 per patient annually. This includes billing for device setup, monthly monitoring, and patient education. To optimize reimbursement rates, organizations must ensure compliance with documentation requirements and invest in training staff to manage RPM workflows efficiently.
3. Engage Private Investors and Philanthropic Funding
Private funding sources, such as healthcare investors and philanthropic organizations, can provide additional financial support for RPM implementation. These entities are often interested in funding innovative healthcare solutions that demonstrate measurable impact. Highlighting the shift from traditional telehealth to proactive RPM models, which utilize advanced monitoring technologies, can attract interest from investors focused on cutting-edge healthcare innovations. For further insights into technology-driven funding approaches, explore ai healthcare investment trends.
4. Partner with RPM Vendors for Cost Sharing
Collaborating with RPM vendors can significantly reduce upfront costs. Many vendors offer flexible pricing models, including subscription-based plans or shared-risk agreements, which align their success with the program’s performance. For instance, vendors like CareSimple provide devices and technical support, enabling healthcare organizations to focus on patient engagement and care delivery. Establishing partnerships with vendors who prioritize long-term collaboration can ensure the program’s scalability and sustainability.
5. Blend Public and Private Funding Streams
Combining public grants with private investments creates a diversified funding portfolio that minimizes financial risk. For example, organizations can use federal grants to cover initial technology costs while relying on private funding for operational expenses and program expansion. This blended approach ensures a steady flow of resources, allowing RPM programs to grow without interruptions.
Checklist for Securing RPM Funding
To streamline the funding process, healthcare organizations should follow this checklist:
- Research federal grant opportunities and prepare compelling applications.
- Ensure compliance with Medicare RPM billing requirements to maximize reimbursements.
- Develop a pitch for private investors that highlights the program’s innovation and impact.
- Negotiate cost-sharing agreements with RPM vendors to reduce upfront expenses.
- Create a funding roadmap that integrates public and private resources for long-term sustainability.
By implementing these strategies, healthcare organizations can establish robust RPM programs that improve patient care while maintaining financial stability.
Vendor Support for RPM Funding
Specialized vendors play a pivotal role in ensuring the seamless adoption of remote patient monitoring (RPM) systems, particularly when it comes to funding strategies. Their expertise spans multiple areas, including pre-award consultations, device selection, technical integration, and long-term sustainability planning. These services are essential for healthcare providers aiming to maximize the benefits of RPM while minimizing operational challenges.
Pre-Award Consultations: Laying the Groundwork
Before funding applications are submitted, vendors often provide tailored consultations to help organizations identify the most suitable RPM devices and programs. This step ensures that funding proposals align with both clinical needs and financial goals, increasing the likelihood of approval.
Device Selection and Technical Integration
Choosing the right RPM devices is critical for program success. Vendors assist healthcare providers in evaluating options based on compatibility, functionality, and cost-effectiveness. Once devices are selected, vendors also facilitate technical integration, ensuring seamless interoperability between RPM systems and existing health data platforms. Analytical data on health data interoperability funding underscores opportunities that are interwoven with the structural needs of remote patient monitoring systems.
Post-Program Sustainability Planning
Beyond implementation, vendors help organizations plan for the sustainability of RPM programs. This includes exploring flexible pricing models such as leasing options or subscription-based platforms, which can ease financial strain over time. Additionally, vendors provide ongoing technical support to ensure systems remain functional and scalable as patient needs evolve.
Conclusion
Sustainable Remote Patient Monitoring (RPM) programs thrive on a well-rounded funding strategy. By integrating federal grants, reimbursements, private funding, and vendor support, healthcare organizations can ensure long-term success. For instance, earlier statistics highlighted the growing reliance on private funding sources, underscoring their role in bridging financial gaps. These strategies not only secure the necessary resources but also enhance patient outcomes through consistent program delivery.
A multifaceted approach to funding is essential to adapt to evolving healthcare needs. Combining diverse financial streams creates a stable foundation, enabling organizations to focus on innovation and patient care.
If you're ready to strengthen your RPM initiatives, we can help. Explore our Fundraising Assistance service for expert guidance on securing capital. Let us assist you in identifying the right funding opportunities to drive your program forward.
Key Takeaways:
- Diverse funding avenues including federal grants, Medicare/Medicaid reimbursements, and private funding are essential for successful RPM implementation.
- Integrating multiple financial streams optimizes revenue generation and enhances patient care.
- Vendor support and strategic partnerships play a crucial role in streamlining RPM adoption.
- Real-world statistics, such as the dramatic increase in Medicare RPM spending, underscore the growth and potential of RPM funding.
Frequently asked Questions
What is remote patient monitoring funding?
Remote patient monitoring (RPM) funding encompasses financial strategies and mechanisms—such as federal grants, Medicare/Medicaid reimbursements, private funding, and vendor partnerships—that are designed to establish and sustain RPM programs effectively.


 Back
Back



